Intraductal papillary mucinous neoplasms (IPMN)
Intraductal papillary mucinous neoplasms (IPMN) were first reported by Ohashi in 1982. They are typically diagnosed in the sitxth decade of life, in both men and women. IPMN are characterized by the proliferation of mucinous cells forming papillary projection within the main pancreatic duct and/or its branch ducts. This results in cystic dilation of the involved ducts, which often contain mucin plugs.
Four histologic epithelial subtypes of IPMN have been described:
- Gastric type
- Intestinal type
- Pancreatobiliary type
- Oncocytic type
IPMN encompass a wide spectrum of biologic behavior, from benign to overtly malignant. The WHO classification includes:
- Benign lesions (low-grade displasia)
- Borderline lesions (intermediate grade/high grade displasia)
- Malignant lesions (invasive carcinoma)
Invasive carcinomas are subclassified, according to their histologic type, into:
- IPMN-tubular carcinoma, arising from gastric and pancreatobiliary epithelium
- IPMN-colloid carcinoma, arising predominantly from intestinal epithelium
- IPMN-oncocytic carcinoma, arising from oncocytic epithelium
From a morphologic standpoint, IPMN are distinguished into three different entities, according to the ductal involvement (Figure 1). This distinction has been shown to have prognostic relevance:
- Main-duct IPMN, involving exclusively the main pancreatic duct. These neoplasms are aggressive, and harbor an situ/carcinoma or invasive carcinoma in up to 70% of resected specimens. The dilation of the main pancreatic duct may be either segmental or may involve the entire duct (panductal IPMN)
- Branch-duct IPMN, involving exclusively the secondary ducts. These neoplasms have a low/medium malignant potential (up to 20-25%), and harbor an invasive carcinoma in up to 10% of resected specimens. Branch-duct IPMN are often multifocal (multiple involvement of brand-ducts).
- Mixed-IPMN, involving simultaneously the main duct and the branch ducts. The biological behavior of mixed-type IPMN is similar to that of main-duct IPMN. The branch-duct component is often multifocal.
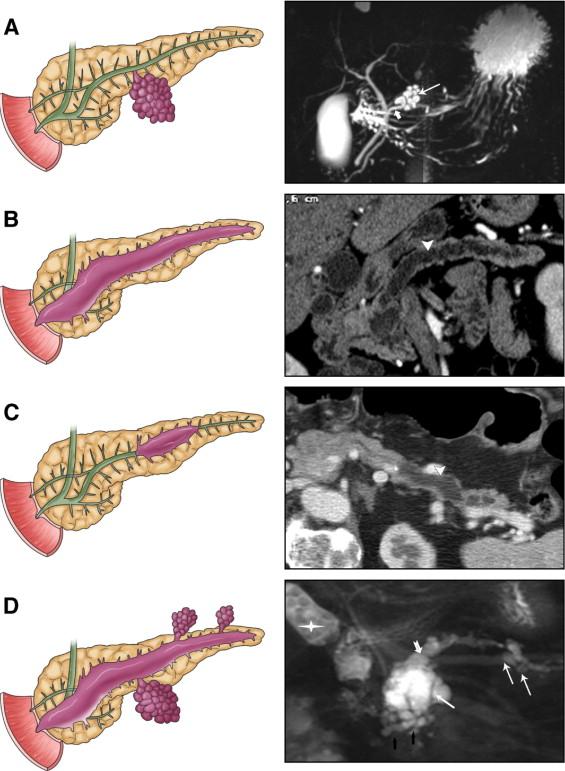 Figure 1. Types of IPMN and correlation with radiologic appearance. A = branch-duct IPMN, B = main-duct IPMN (panductal), C = main-duct IPMN (segmentary), D = mixed IPMN. Copyright Chirurgia del Pancreas Verona.
Figure 1. Types of IPMN and correlation with radiologic appearance. A = branch-duct IPMN, B = main-duct IPMN (panductal), C = main-duct IPMN (segmentary), D = mixed IPMN. Copyright Chirurgia del Pancreas Verona.
The most recent guidelines for the management of pancreatic mucin-producing neoplasms (International Association of Pancreatology 2012) defined radiologic “worrisome features” or “high-risk stigmata” to stratify the risk of malignancy (especially in branch-duct IPMN):
Worrisome features
- Cyst of >3 cm
- Thickened enhanced cyst walls
- Non-enhanced mural nodules
- Main pancreatic duct size of 5-9 mm, or abrupt change in the main-pancreatic duct caliber
- Lymphadenopathy
High-risk stigmata
- Enhanced solid component
- Main pancreatic duct size of >10 mm
All cysts with worrisome features should be evaluated by endoscopic ultrasound to further risk-stratify the lesion. If non-operative management is chosen, the surveillance should be strict. Cysts with obvious high-risk stigmata on cross-sectional imaging should undergo resection without further testing. All patients with cysts without worrisome features should undergo surveillance.
Nowadays, IPMN are the most frequent cystic neoplasm of the pancreas. Small, asymptomatic branch-duct IPMN are being increasingly diagnosed, and radiologic and autoptic studied indicate that the prevalence of IPMN in the elderly (>65 years) is nearly 10%.
Another relevant issue is the association between IPMN and pancreatic and extra-pancreatic carcinogenesis. In other words, patients with IPMN seem to have a greater risk of developing an extra-pancreatic neoplasm of a metachronous pancreatic carcinoma. However, this notion comes from a very small number of prospective studies, but strict adherence to well-established screening protocols for cancer is advised in these patients.
Click on the following links for more information about main-duct/mixed IPMN and branch-duct IPMN.
Main-duct/mixed IPMN
Branch-duct IPMN
Learn more:
Sakorafas GH et al. Surg Oncol. 2011;20:109-118.













